Therapists with Zencare's Private Pay Booster can verify client benefits, and their clients can file out-of-network claims through the Reimbursify app.*
Share this article with clients to teach them how to file out-of-network claims (and get reimbursed for therapy!).
Here's how to file out-of-network claims as a client:
1. Download the Reimbursify app to your smartphone.
2. Create your account by entering your contact information and insurance details.
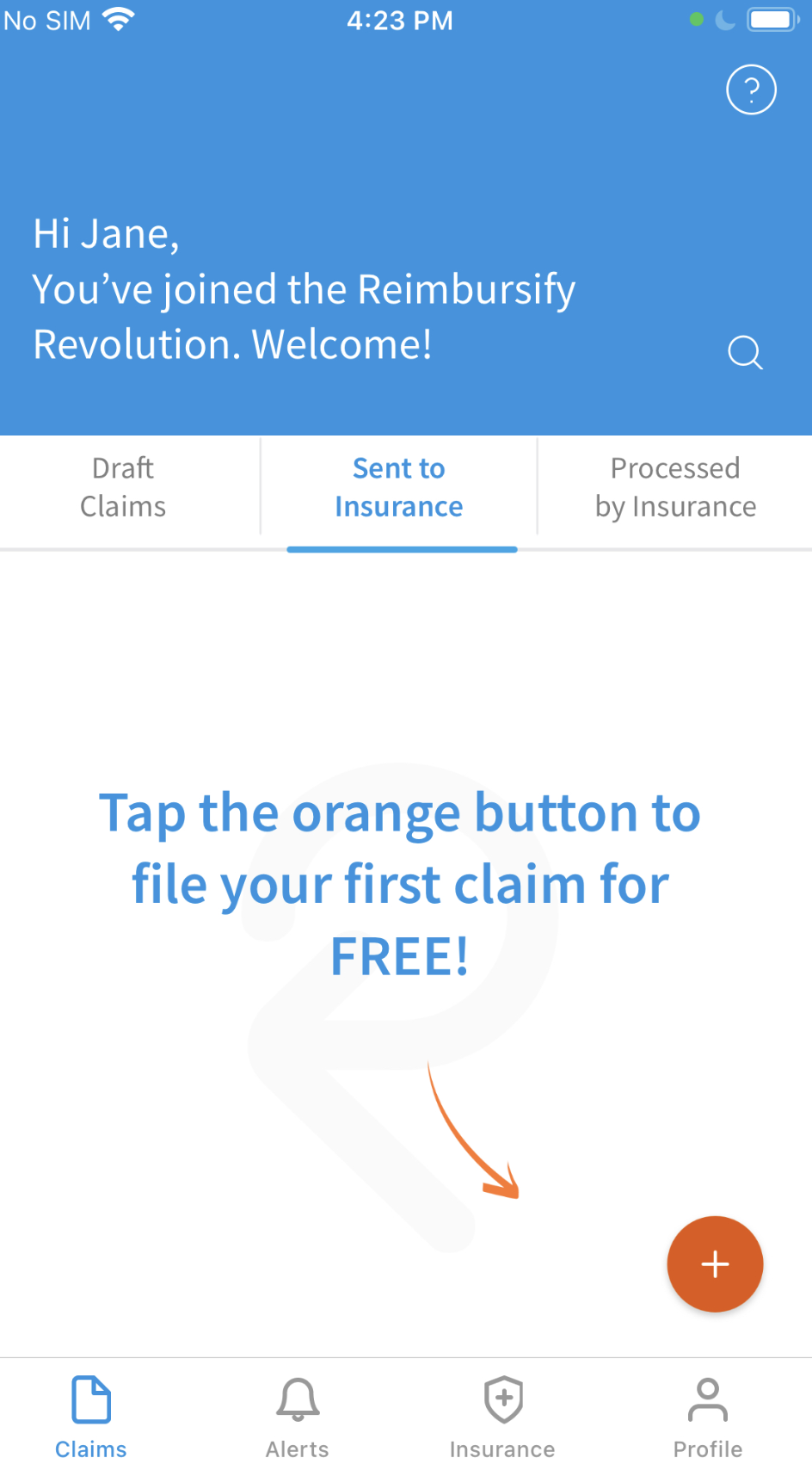
3. Create your first claim by clicking the orange plus button.
4. Add a patient. Tap the name of the patient who received the treatment for this claim. Tap "Add a new family member" to add a new patient to your account.
5. Choose a date. Choose dates on the calendar to specify when the visit(s) took place. You can select multiple dates if all of the visits had the same codes and fees.
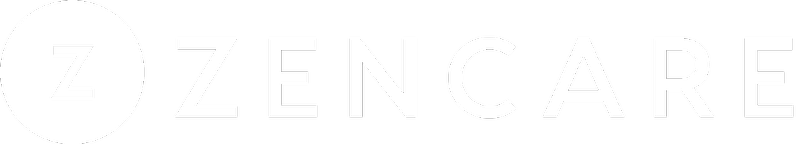
6. Submit a photo of your superbill. Tap the orange shutter button to take a photo of your receipt/superbill, or tap the upload icon to select a digital file (PDF) from your phone. Use the cropping tool to select only the portion of the photo that contains your receipt/superbill. You can submit multiple photos if you are submitting claims for more than one visit.
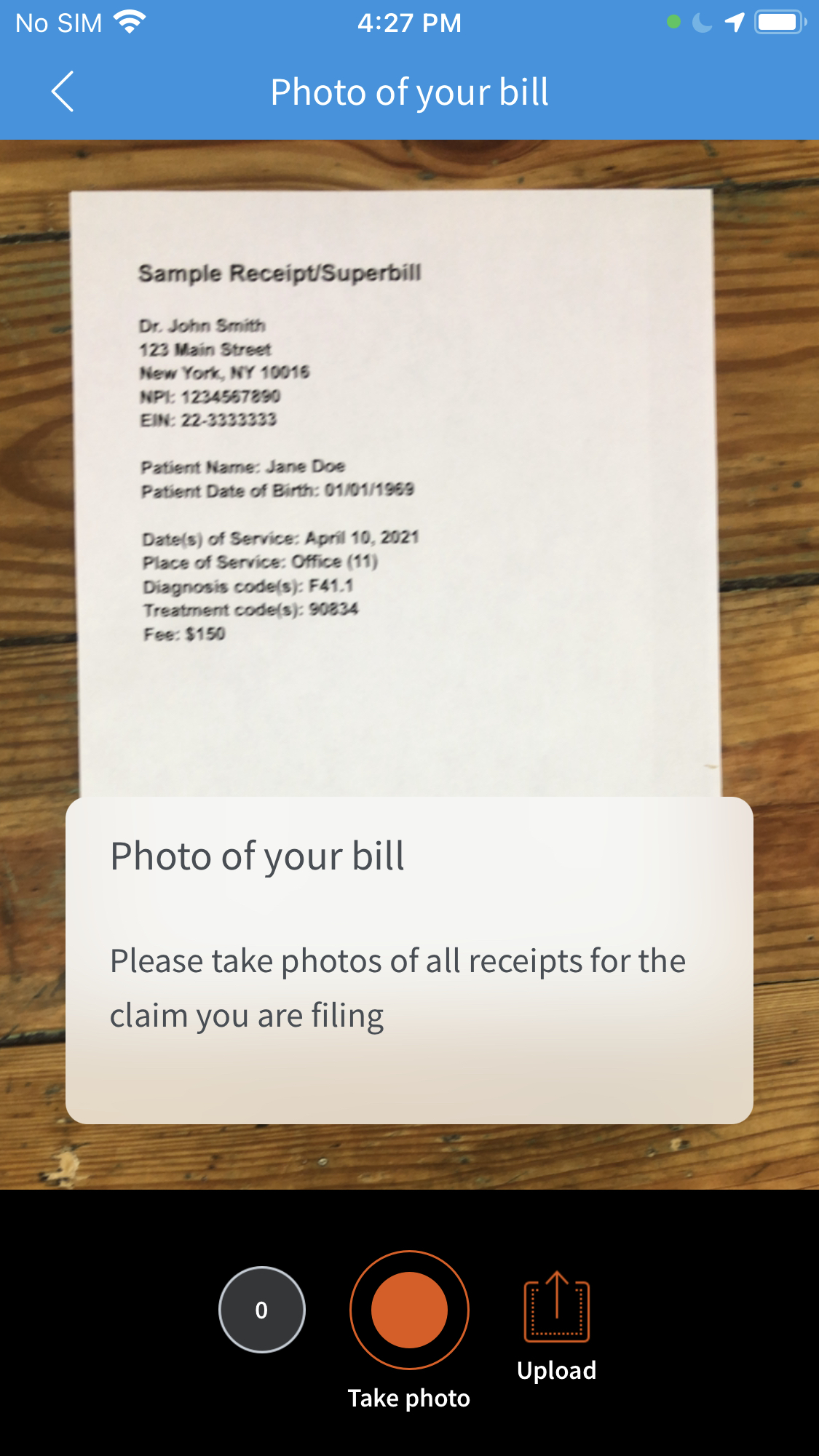
7. Add a practitioner. Tap the name of the therapist or psychiatrist who provided the treatment for this claim. Tap "Add a new Practitioner" to add a new practitioner to your account.
Note: If your practitioner is not in the Reimbursify system, it will be necessary to add your practitioner’s Tax ID to the claim. This is a one-time step. Your practitioner’s Tax ID can be found on your receipt/superbill. They are sometimes referred to as EIN numbers, and have nine digits, i.e., “12-3456789”.
8. Enter the diagnostic code. Tap into the "Diagnosis Code" field to enter the diagnosis code(s) for this claim. Diagnosis codes can be found on your receipt/superbill. They are sometimes referred to as "ICD-10" codes or "DX" codes and usually start with a letter, i.e., "F41.1" or "G47.00." Tap the orange "Add" button after you have typed a code, to add it to the claim. Tap the orange "Continue" button when you have added all of the diagnosis codes for the visit.
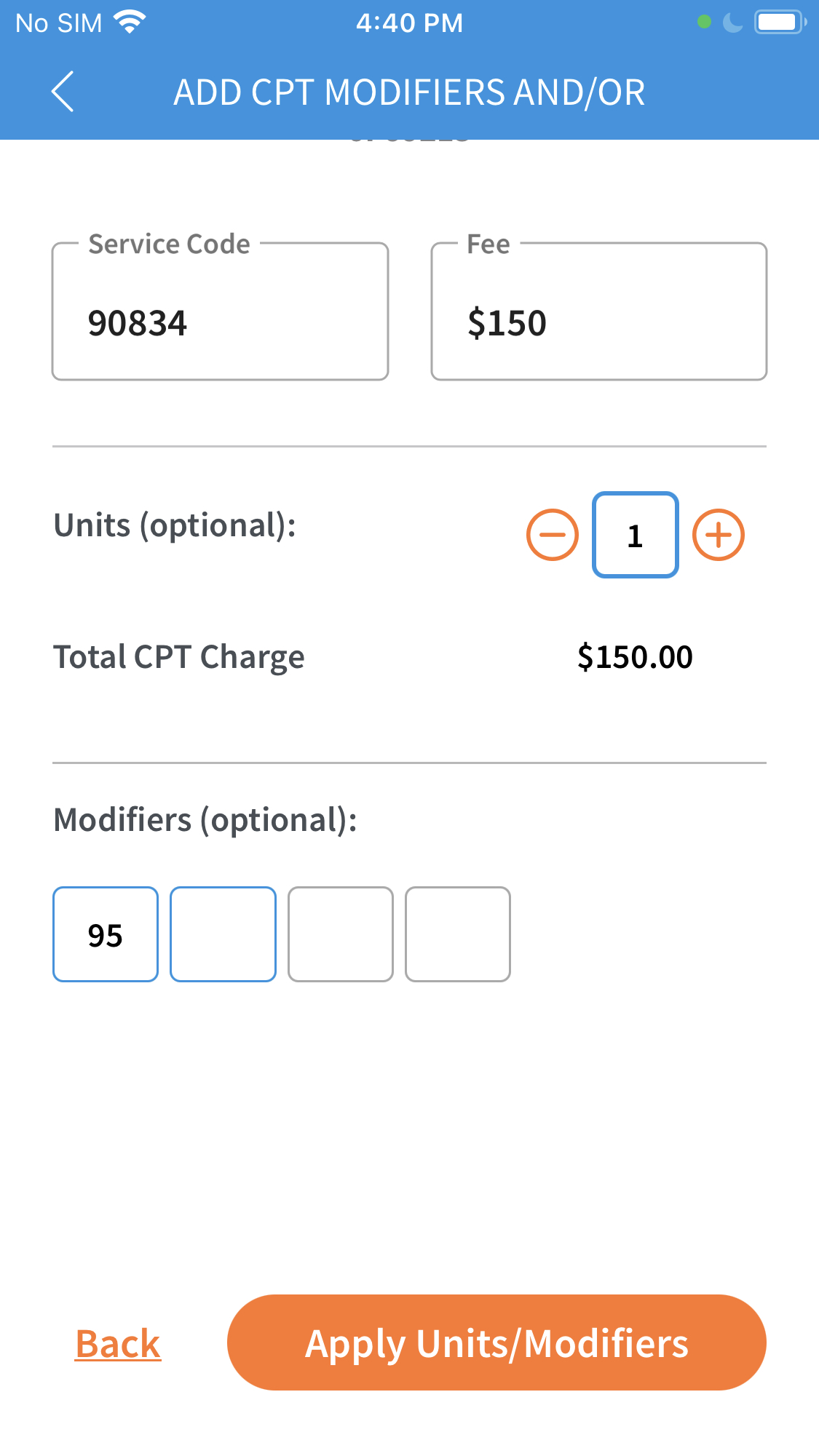
9. Enter the Service Code. Tap into the "Service Code" field to enter the service code(s) for this claim. Service codes can be found on your receipt/superbill. They are sometimes referred to as CPT, treatment codes or procedural codes and are always five digits, i.e., "90834" or "99213." Tap into the "$Fee" field to enter the fee associated with each treatment code. The fee should include any discounts that were applied to your bill. Tap the orange "Add" button after you have typed a code, to add it to the claim. Tap the orange "Continue" button when you have added all of the service codes and fees for the visit.
Select the checkbox below the Service Code field to apply modifiers or units. Modifiers indicate that the treatment was altered by some specific circumstance, when that circumstance is not defined by a different code, and are common with certain types of treatments, like telehealth visits (modifier "95"). Units are common with physical therapy visits, where treatments can be applied in 15-minute increments. Tap the orange "Continue" button after you have typed a code, fee and any applicable modifiers or units.
10. Review the details of your claim, and then tap the orange "Submit" button to send it to your insurance company. (Note: If this is not your first claim, you may have enter payment details in order to submit the claim.)
11. That's it! Your claim is on its way to your insurance company, and you will receive an email from Reimbursify confirming your submission.
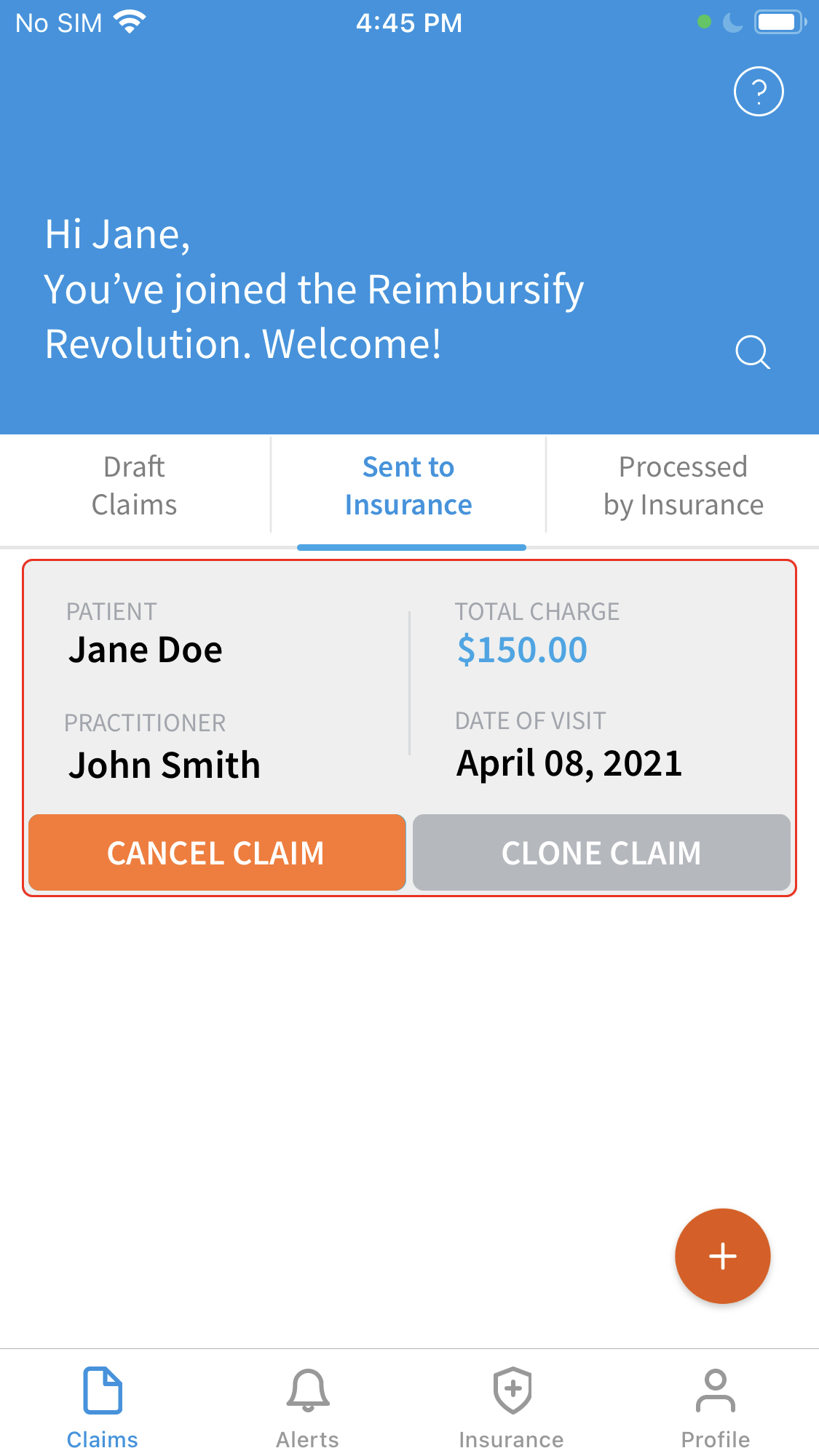
You can view the status of your claim at any time by selecting the "Sent to Insurance" tab on the Claims dashboard.
It typically takes 30-45 business days for most insurance companies to process claims, after which time you will receive an Explanation of Benefits (EOB) in the mail or via email, containing details about which portion of your visit is covered by your plan, how much was applied to your deductible and how much was reimbursed. You can enter these details for any claim under the "Processed by Insurance" tab on the Claims dashboard.
*With Zencare's Basic Private Pay Booster, clients pay $3.99 per claim filed. Professional and Premium tiers allow clients to file claims for free.